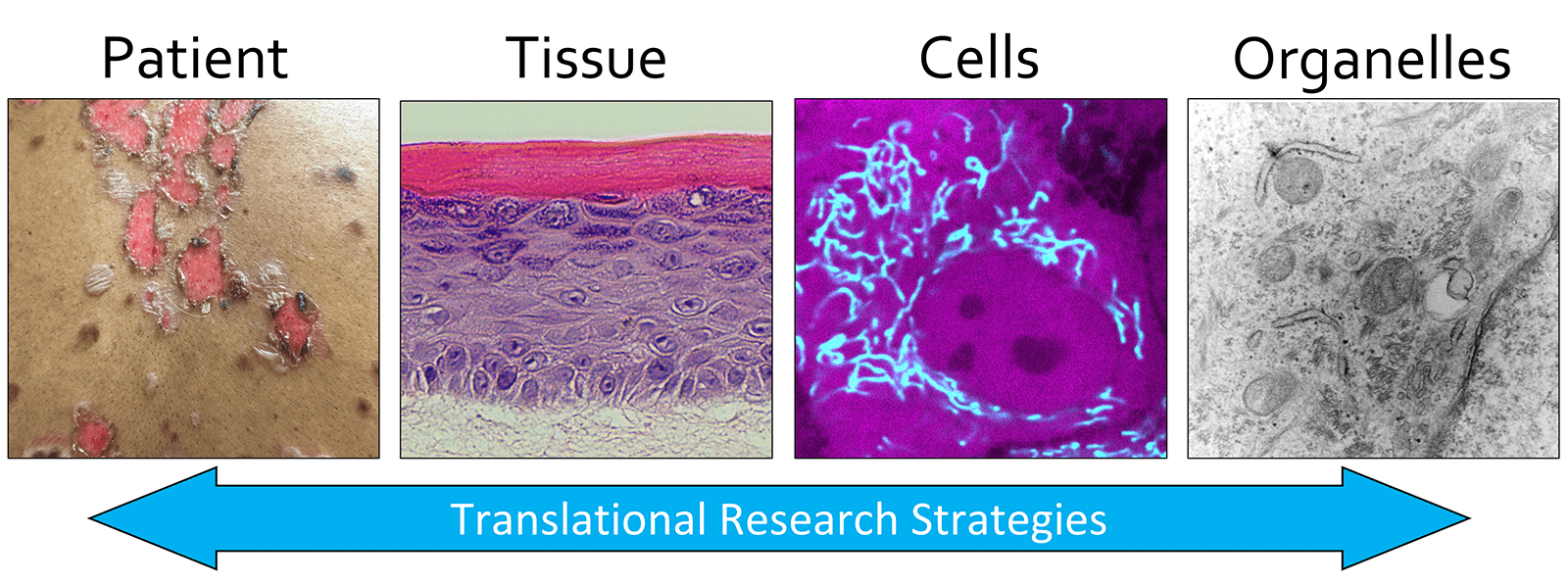
Overview
Our lab studies the skin, which protects the body from infection and dehydration. We focus on how skin cells called keratinocytes mature to form an effective barrier tissue and how this tissue falls apart in skin fragility diseases that cause chronic blistering and painful wounds. Our ultimate goal is to identify novel approaches to promote skin tissue regeneration and to uncover new treatments for rare genetic skin blistering disorders, many of which lack any FDA-approved therapy. Our current projects focus on Darier disease, Hailey-Hailey disease, ichthyosis, psoriasis, and epidermolysis bullosa (EB).
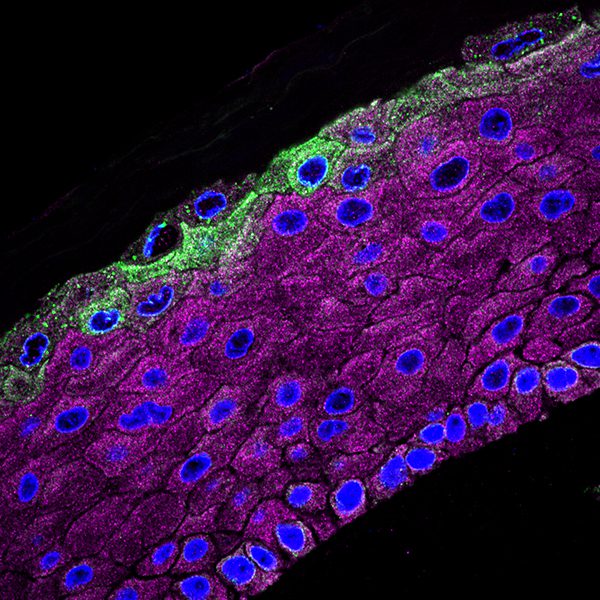
Keratinocyte Cell Biology
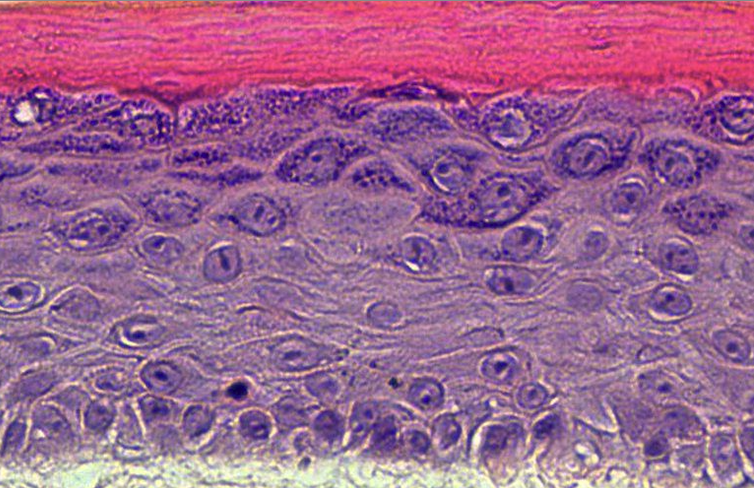
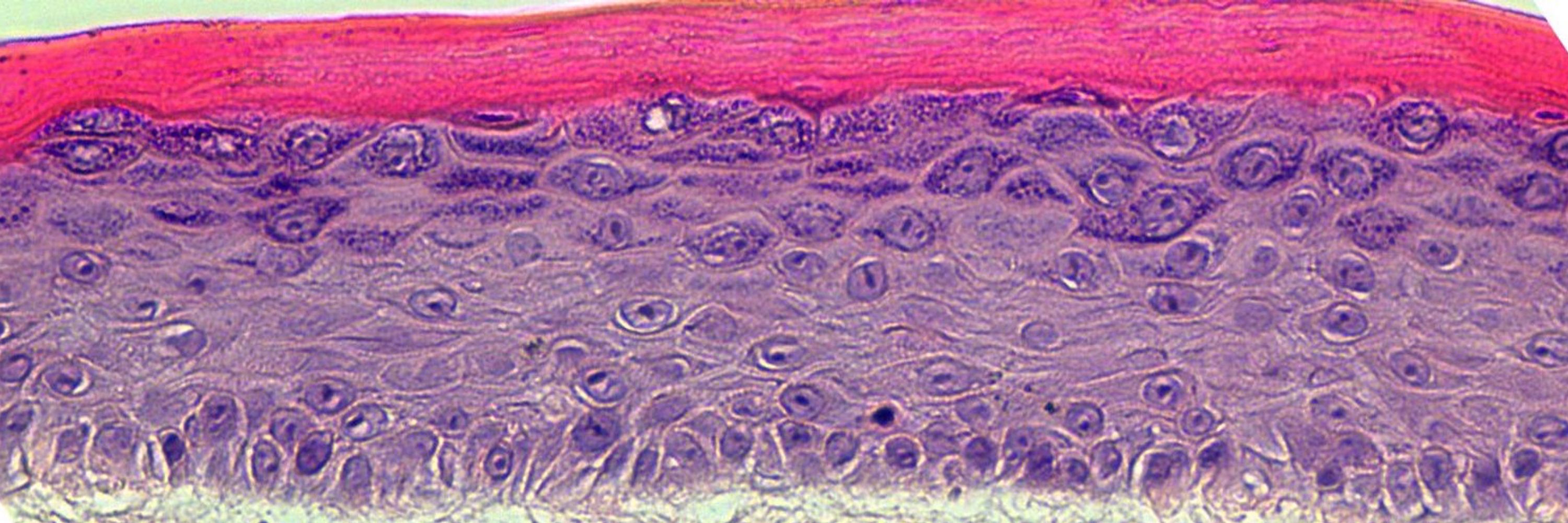
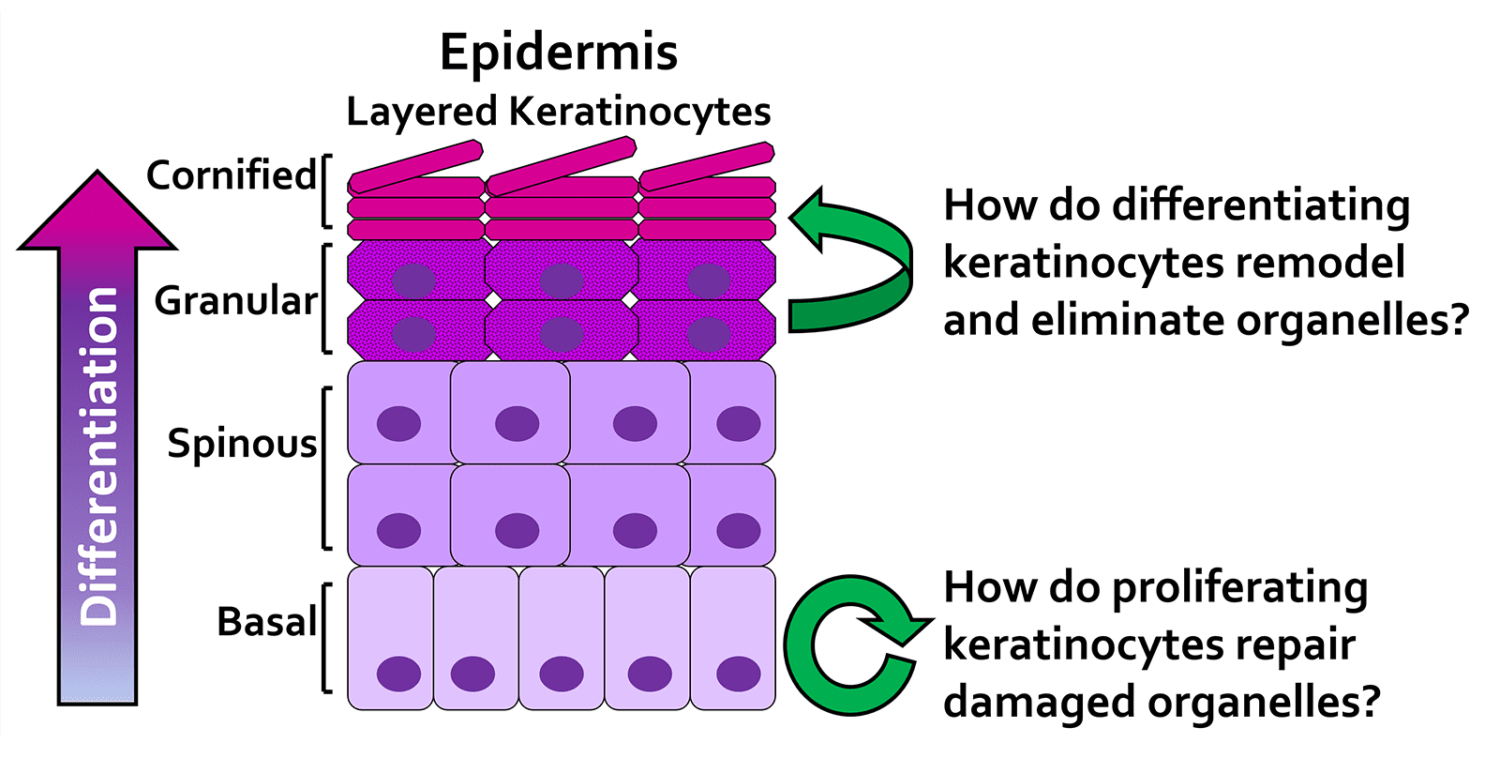
The outermost layer of the skin, the epidermis, is made up of multiple layers of cells called keratinocytes that form a protective barrier for the body. Keratinocytes continually replicate themselves to replenish the skin tissue as it is naturally shed every month and undergo a process of maturation to strongly adhere to one another to resist wounding. This biology is disrupted in common human skin diseases like eczema and psoriasis and in rare genetic skin fragility disorders like ichthyosis, Darier disease, Hailey-Hailey disease, or epidermolysis bullosa (EB). Our limited understanding of the fundamental biology of how keratinocytes mature and stick together has prevented development of effective therapies to promote regeneration of the epidermis after wounding or for treating patients with genetic skin disorders.
Epidermis Diagram
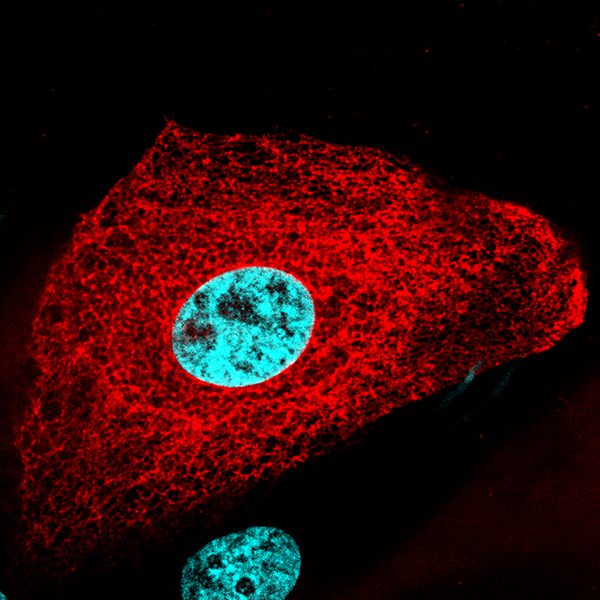
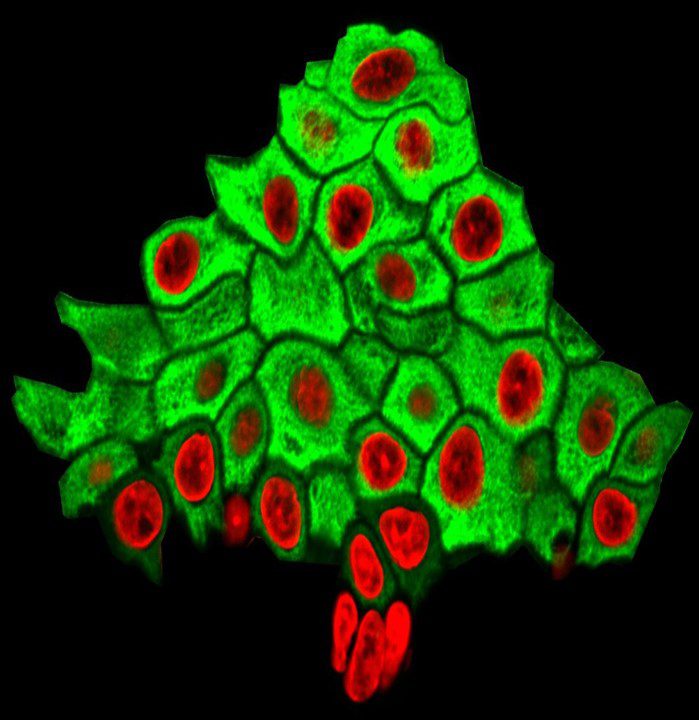
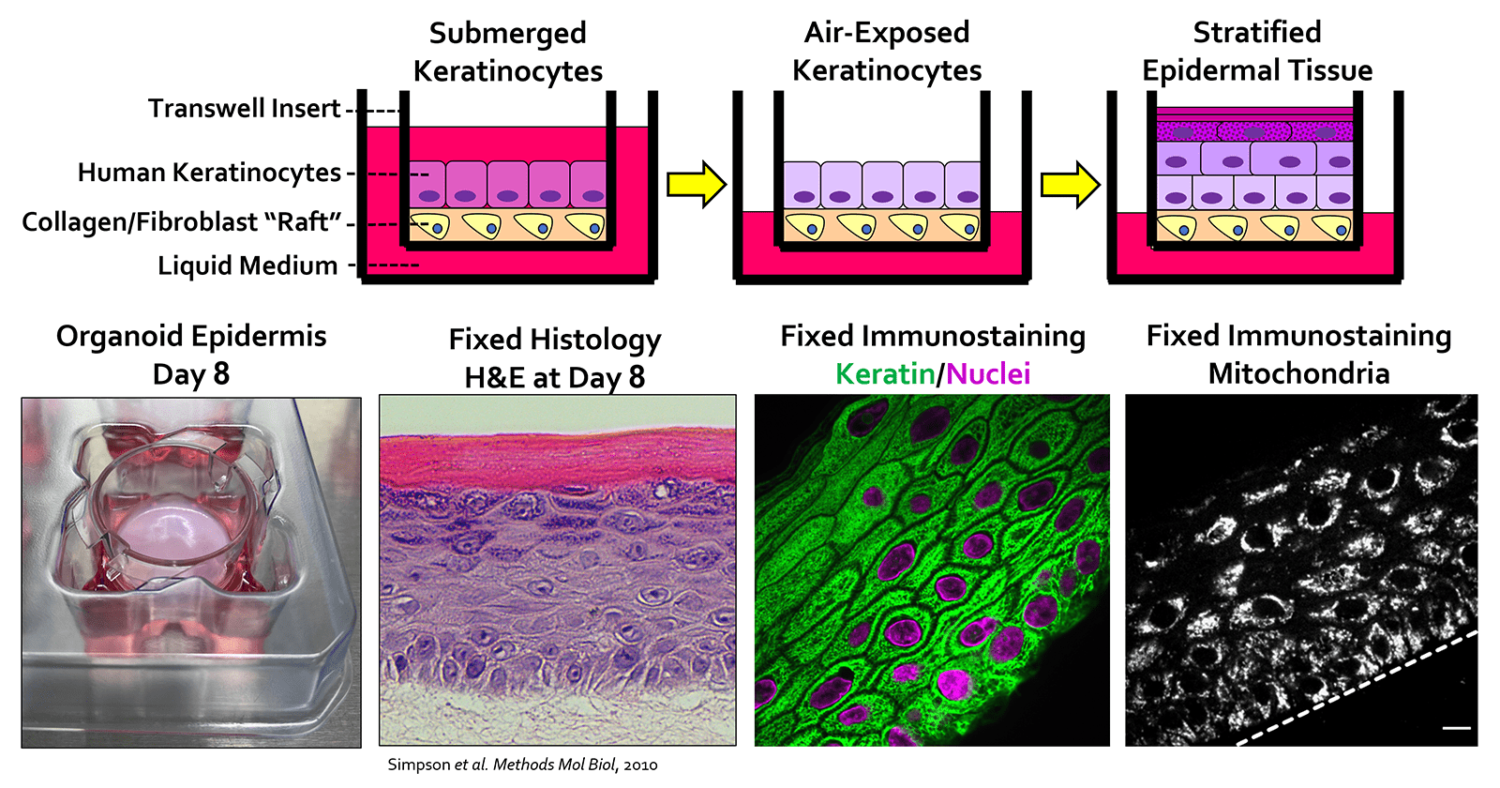
Organoid Skin Imaging
Our lab has developed an “organoid” model of the skin in which human keratinocytes form a multi-layered epidermal tissue in just one week. Coupling this system with high-resolution imaging techniques, like confocal microscopy, permits us to visualize changes in the live organoid skin model as it is developing into a mature tissue. We can engineer human keratinocytes to express fluorescent proteins that are visible using a high-magnification microscope allowing us to visualize these cells at the level of single organelles (e.g., mitochondria) to better understand how the epidermis forms.
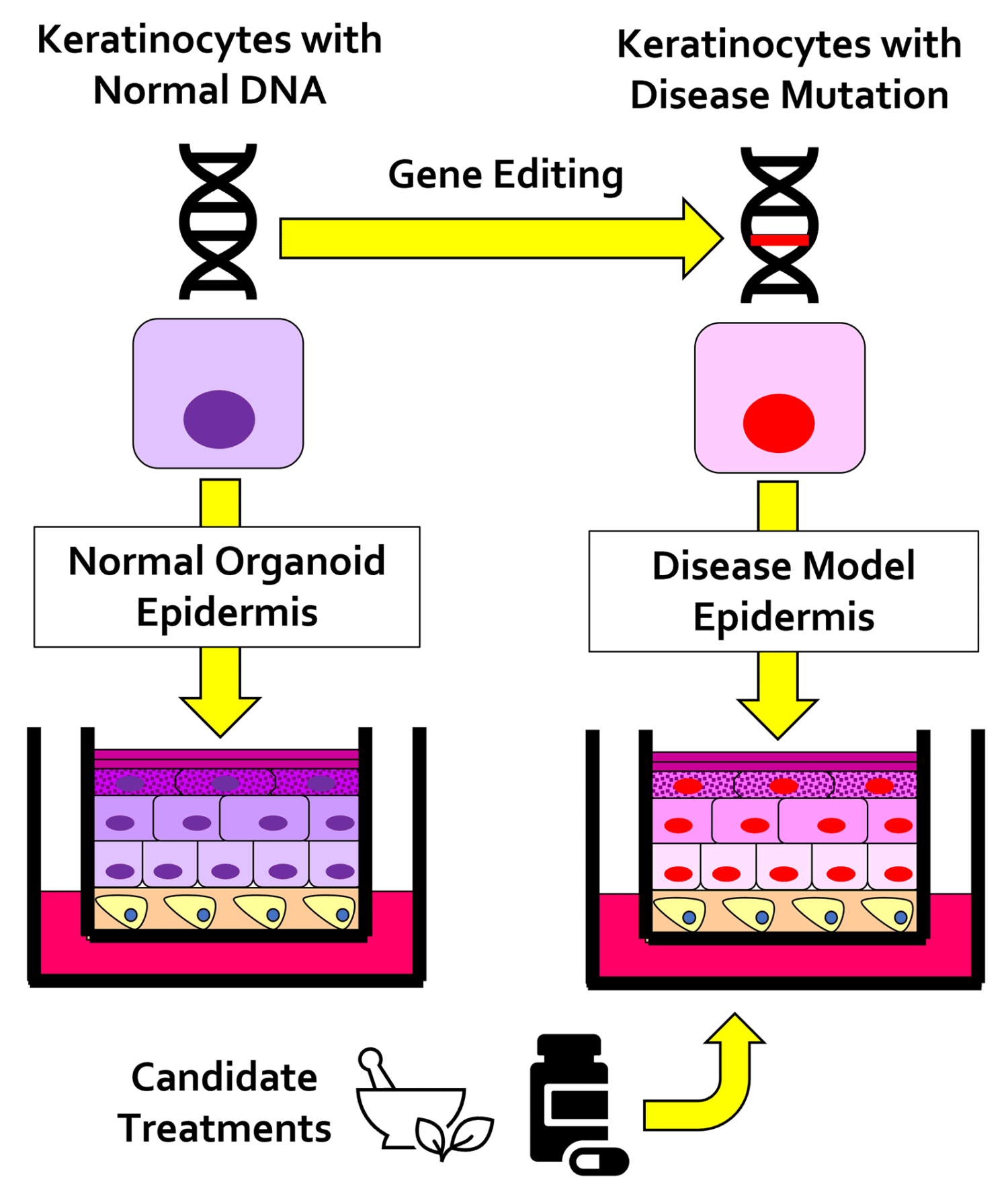
Gene Editing in the Skin
We use gene editing techniques (e.g., CRISPR/Cas9) in human keratinocytes to introduce DNA mutations linked to skin disorders. By culturing these engineered cells in the organoid system, we are able to replicate skin tissue pathology in the lab. These 3-D models of skin disease can be used for high-resolution imaging to better understand what causes the disease and for testing new treatments. Our ultimate goal is to identify novel therapies to promote tissue regeneration after skin injuries and to restore epidermal barrier function in inherited and currently incurable dermatologic diseases.